Proximal Humerus Fracture Fixation.
Why might I need proximal humerus fracture fixation?
Not everyone with a fractured proximal humerus needs fixation. If possible, Mr Moverley will treat your fracture with non-operative treatments, like pain medicines, physiotherapy, and slings. You may benefit from proximal humerus fracture surgery in the following scenarios:
Dislocated fractures, in which the humeral head (the ball) has dislocated from the shoulder socket.
Open fractures, in which the bone penetrates the skin.
Injuries to surrounding blood vessels and nerves.
Humeral head-split fractures, in which a portion of the humeral head breaks and disrupts the cartilage of the joint.
Widely displaced fractures in younger or high demand patients.In these cases, fixation can realign your bones back into their proper configuration. This significantly increases the chance that your bone will heal properly and may be associated with improved long-term function.
What does surgery involve?
On the day of surgery you will be admitted to the ward or surgical admission area. You will once again meet Mr Moverley who will ensure you are still happy to proceed and that you understand the risks and benefits of the procedure. This is a good opportunity for you to ask any further questions. You will be asked to sign a consent form if you have not already done so.
You will meet your anaesthetist who will explain the type of anaesthetic you will receive. Most proximal humerus fracture surgery requires a general anaesthetic (you will be asleep) and a nerve block so that the arm will be numb for approximately 12 hours post operatively.
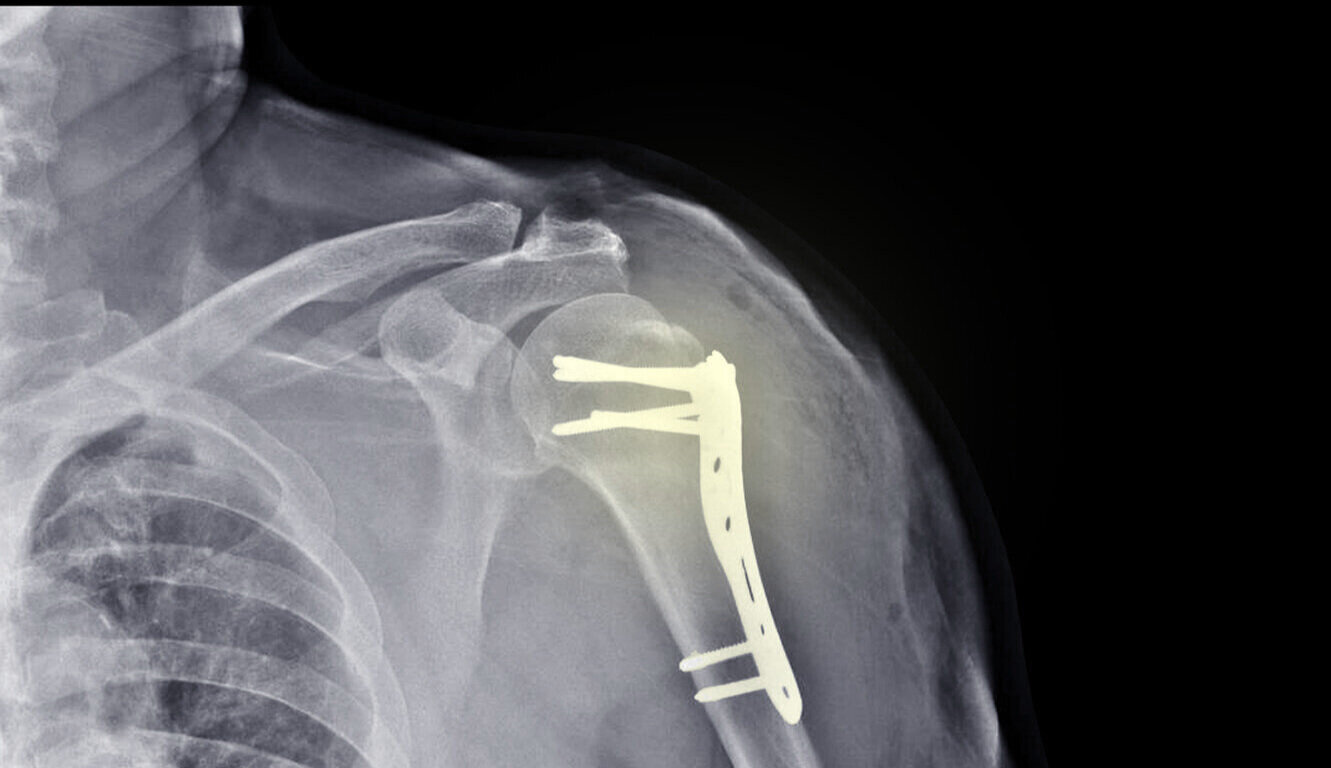
Surgery is performed through an open incision on the top of the shoulder. The length of the scar will depend on your fracture configuration but 10-15cm is typical. During your operation, the fracture is realigned and then fixed in place with a plate and screws.
The specific technique will depend on the exact fracture configuration; the ultimate goal is that the normal shoulder anatomy is restored as closely as possible. The wounds are repaired with stitches and covered with a splash proof dressing. The wounds should be kept dry for 10-14 days.
Occasionally the broken bones cannot be reconstructed and in this case a shoulder replacement will be needed.
What happens post operatively?
Immediately after surgery your arm will be in a sling. You will be given painkillers if you are in any pain, and these will also be provided upon discharge.
A physiotherapist will assess you to make sure that you can remove and apply the sling safely. They will provide some early exercises to help prevent stiffness of the hand, wrist and shoulder.
How long is the rehabilitation process?
A sling will be provided to rest the shoulder but this should usually only be used for the first few weeks after surgery. Early shoulder movement is encouraged to prevent stiffness.
Physiotherapy is individualised to your specific needs and will progress with the following goals:
Early (1-2 weeks): Minimize post-operative stiffness with active finger, wrist and elbow movements. Shoulder pendulum exercises progressing to full active range of movement as pain allows.
Middle (2-6 weeks): Continue to progress towards full active range of movement
Late (6-12 weeks and beyond): Strengthening program, once full range has been achieved. Graded return to all previous functional and recreation activities after 12 weeks.
Approximately how long will it be before I can...?
Drive: 6 weeks
Desk job: 2 weeks
Manual work: 12-16weeks
Golf: 12 weeks
Racket sports: 16 weeks
Repetitive overhead activity: 16weeks
Pain and stiffness can persist for 9-12months post operatively.
What are the potential risks and complications?
As with any operation, a small number of people may have problems after proximal humerus fracture fixation. Most of these problems are quite minor and can be treated easily but in approximately 5-10% of cases, further surgery is needed. The main risks are:
Infection (1-2% of cases)
Major bleeding
Nerve injury
Avascular necrosis and shoulder arthritis
Shoulder stiffness (frozen shoulder)
Numbness around the surgical scar
Symptomatic metal-work requiring removal (5-10% of cases)
Is proximal humerus fracture fixation always successful?
Proximal fracture fixation leads to a healed bone in over 95% of cases. The overall complication rate is approximately 5-10%. While these statistics are encouraging, the results of proximal humerus fracture fixation are therefore not guaranteed which is why Mr Moverley will want to discuss possible non-operative measures with you before proceeding.